Medical myths matter. All of our decisions, although they often seem small to us in the middle of a busy shift, have real impacts on people’s lives. To be a truly expert clinician, you have to understand not just what to do, but why you are doing it.
The primary myth covered in this talk was the use of topical anaesthetics in the management of simple corneal abrasions. The full handout and list of articles can be found here.
I also covered Salter-Harris 1 injuries, the myth that ligament is stronger than bone, and that concept that not all of these injuries need a cast. A full handout with references on the topic can be found here.

If you are interested, a few of the other medical myths that I mentioned during the talk were:
The use of PPIs for upper GI bleeds
The benefit for stress testing in low risk cardiac patients
As physicians, we are trusted sources of medical information. We are relied upon not just by our patients, but also our families and friends to be knowledgeable and credible sources of information about health. We should all probably be aware of common medical myths, such as the need to drink 8 glasses of water a day, the idea that we only use 10% of our brains, or the thought that eating turkey might make you sleepy, because even these seemingly benign misunderstandings can have tremendous impacts on people’s lives. For a short, fun read on some of these topics, see:
Vreeman RC, Carroll AE. Medical myths. BMJ (Clinical research ed.). 335(7633):1288-9. 2007. PMID: 18156231 [free full text]
Charles Sidney Burwell, the dean of Harvard medical school at the time, famously said, “Half of what we are going to teach you is wrong, and half of it is right. Our problem is that we don’t know which half is which.” This may still be true today, but I don’t think this has to be true. If we taught the complexity of science, rather than just a collection of facts, we wouldn’t be wrong. We would understand the need for replication of studies and the limitations of p values. We would be able to differentiate treatments with great evidence (ASA in MI) from those with bad evidence (tamsulosin for renal colic), and we wouldn’t be so surprised by the constant updates that are part of the normal scientific process.

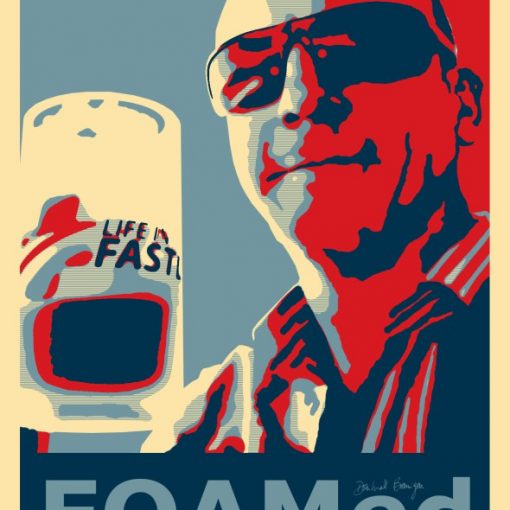
There is a lot of evidence to keep track of and not many of us are laden with free time. How is one supposed to keep up with everything? In this day and age, I think the answer is crowdsourcing the work. There are so many great, free EBM resources available not that I don’t think there is any excuse in falling behind. This handout covers my favourite sources of evidence based medicine and critical appraisal.

If anyone takes up my challenge and finds an interesting answer while exploring why we do what we do, feel free to contact me and we can share it here with everyone else. You can use this contact page or else e-mail me at first10em at gmail dot com.