In addition to the critically appraised topic in part 1, here are some additional papers on stress testing worth knowing about.
First, I updated the original search using the same search parameters to look for new papers. There were no new papers that would have fit the original inclusion/exclusion criteria, so if I was repeating the project today, I would still submit the same final paper. The only relevant paper I could find did not have any MIs or deaths in their 30 day follow up:
Napoli AM. The association between pretest probability of coronary artery disease and stress test utilization and outcomes in a chest pain observation unit. Acad Emerg Med. 2014;21:(4)401-7. PMID: 24730402
- A prospective observational cohort of 3553 patients admitted to a chest pain unit
- Low risk patients, with non-dynamic ECGs and negative troponins
- 1754 (49%) had a stress test
- Only 20 (1.1%; or 0.6% of total group) were called true positive, but that definition is based only on angiogram, not subsequent outcomes
- 9 (0.6%) were called false positives
- No patients who were defined as low risk (using a D&F score) had a true positive stress test or bad outcome
Bottom line: Exercise stress testing has an extremely low yield, even for softer outcomes. Again, there were no MIs or deaths at 30 day follow-up.
Although death and MI are the major outcomes I think that we should be focusing on in the emergency department, some people argue that we should also be practicing primary care and trying to diagnose coronary artery disease. So we should ask:
How good is exercise stress test at detecting coronary artery disease?
Froelicher VF, Lehmann KG, Thomas R, et al. The electrocardiographic exercise test in a population with reduced workup bias: diagnostic performance, computerized interpretation, and multivariable prediction. Veterans Affairs Cooperative Study in Health Services #016 (QUEXTA) Study Group. Quantitative Exercise Testing and Angiography. Ann Intern Med. 1998;128:(12 Pt 1)965-74. PMID: 9625682
- 814 consecutive patients with angina (so exactly the kind of patient we would discharge from the ED) underwent both exercise stress test and angiography
- This is the only large study I know of where all patients underwent the gold standard of angiography after a stress test. (Gold standard for anatomical disease.)
- Using angiography as a gold standard, exercise stress testing had a 45% sensitivity and an 85% specificity
Bottom line: Stress testing is very poor at identifying anatomical disease. These numbers are especially bad when you try to apply the test to a group with a very low pre-test probability of disease. (Using a sensitivity of 45% and a specificity of 85%, the positive likelihood ratio of stress testing is 3, while the negative likelihood ratio is 0.65)
Does stress testing stable patients change outcomes?
So stress testing does not identify patients at short term risk of MI or death. Based on the last study (which is consistent with all the literature) it also appears to be pretty bad at identifying CAD. Might it somehow overcome this poor sensitivity and specificity to guide practice and help patients?
There is one RCT that looks at whether a stress test in stable patients with type 2 diabetes (so moderate risk patients) changes long term outcomes:
Young LH, Wackers FJ, Chyun DA, et al. Cardiac outcomes after screening for asymptomatic coronary artery disease in patients with type 2 diabetes: the DIAD study: a randomized controlled trial. JAMA. 2009;301:(15)1547-55. PMID: 19366774
- This is an RCT of 1123 patients with type 2 diabetes randomized to either stress radionuclide myocardial perfusion or no screening
- At 5 years: 7 nonfatal MIs and 8 cardiac deaths (2.7%) occurred among the nuclear stress test group and 10 nonfatal MIs and 7 cardiac deaths (3.0%) among the untested group
- There were no changes in long term outcome whether or not patients were tested
Bottom line: Testing stable patients with a low to moderate risk of CAD with cardiac stress imaging does not prevent deaths or MIs.
The other outcome that some people hope to change by performing stress testing is PCI. The argument is that stress testing will identify the patients that require angiography and PCI, which is the definitive treatment these patients require. However, it is worth asking if the cath lab is likely to help these patients, who (in order to get discharged) had negative ECGs and troponins.
Outside of patients with a STEMI, what is the benefit of angiography in ACS?
This is an important question when you are discussing stress testing, because one of the clear outcomes of sending all chest pain patients for stress tests is that a lot of them end up getting further cardiac testing, including angiography. From the world view that more testing is always better, this seems fantastic. However, does this really work in the real world?
In NSTEMI/Unstable Angina
Hoenig MR, Aroney CN, Scott IA. Early invasive versus conservative strategies for unstable angina and non-ST elevation myocardial infarction in the stent era. Cochrane Database Syst Rev. 2010;(3)CD004815. PMID: 20238333
- Cochrane review of invasive versus conservative strategy in unstable angina and NSTEMI
- No change in mortality overall
- In patients with positive troponins, there is a small benefit in preventing future MIs
- In patients with negative troponins, there is increased mortality with the invasive strategy
Bottom line: This is one of multiple meta-analyses, which all vary a little but, but the general conclusions seem to be the same. Stenting outside of the context of STEMI does not change mortality. In patients with positive troponins, there may be a small benefit. That is countered by increased harm in patients with negative troponins.
In stable coronary artery disease
Boden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:(15)1503-16. PMID: 17387127
- 2,287 patients with documented myocardial ischemia and angiographically confirmed CAD (85% had positive stress tests)
- Randomized to medical therapy versus PCI
- No change in the composite of death, MI, or stroke RR 1.05; 95% CI, 0.87 to 1.27; P=0.62
- No change in MI 1.13; 95% CI, 0.89 to 1.43
- No change in hospitalizations for ACS 1.07; 95% CI, 0.84 to 1.37; P=0.56
Stergiopoulos K, Brown DL. Initial coronary stent implantation with medical therapy vs medical therapy alone for stable coronary artery disease: meta-analysis of randomized controlled trials. Arch Intern Med. 2012;172:(4)312-9. PMID: 22371919
- Meta-analysis of 8 RCTs trials (7229 patients) comparing invasive management versus medical therapy for stable CAD
- No change in mortality OR 0.98 95% CI 0.84-1.16
- No change in non-fatal MI OR 1.12 95% CI 0.93 – 1.34
- No change in unplanned revascularization OR, 0.78; 95% CI, 0.57-1.06
- No change in persistent angina OR, 0.80; 95% CI, 0.60-1.05
Bottom line: You are not helping your patients with CAD by getting them to the cath lab.
How often do we miss ACS in the emergency department?
One final topic is worth covering. Normally, when I get to this point in the conversation, people get pretty worried. We have all been taught that we are going to miss 2% of MIs, and therefore it is very important that we get our patients the stress test so that another doctor will see them before that MI happens. However, the study on which the 2% figure is based actually paints a very different picture:
Pope JH, Aufderheide TP, Ruthazer R, et al. Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med. 2000;342:(16)1163-70. PMID: 10770981
- This is the article that says we have a 2% miss rate and that patients are twice as likely to die if you miss them, however what it actually says is:
- Out of 10,689 patients prospectively evaluated for MI (with a 17% rule in rate)
- 19 patients were discharged home and ultimately diagnosed with MI (0.17%)
- 22 more patients were discharged home and ultimately diagnosed with unstable angina (0.20%)
- In total, this would be a miss rate of 0.38% – and that includes the subjective diagnosis of unstable angina
- 2% gets quoted because 2% of the subset of patients who were ultimately diagnosed with MI that were sent home. However, that is not 2% of the patients we actually see (undifferentiated patients arriving with chest pain).
- The mortality was identical whether your MI was diagnosed in the ED or missed (10.5% versus 9.7%, RR 1.1 95% CI 0.3-4.1)
Bottom line: The rate of missed MI (or ACS) in undifferentiated chest pain patients who we decide to discharge home is actually VERY low (0.2 – 0.38%). It is very unlikely that you are going to be able to make that number better, even with an incredibly good test.

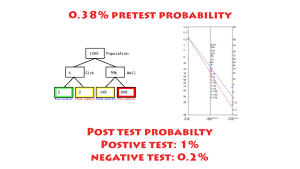
In a population with a missed ACS rate of 0.38%, how well can stress testing possible perform? Well, in the first handout – we saw that it had a sensitivity of 0% for the outcomes we really care about, death and MI. However, lets be generous and assume we would like to identify the CAD that is the risk factor for these 0.38% of misses. In that case, the sensitivity is 45% and the specificity is 85%, leading to a LR- of 0.65 and a LR+ of 3. If we plug those numbers into everyone’s favorite Fagan Nomogram, our post-test probabilities would be:
- After positive test: 1% 95% CI 0-3%
- After negative test: 0.2% 95% CI 0-1%
Not only are these numbers clinically useless, the accuracy of the estimates overlap. The test cannot distinguish between patients.
(This math is not technically correct, as we are using the LRs for CAD, but the prevalence of ischemia. We already know that stress testing doesn’t pick up ischemia, so I am looking at it like it is actually used in the ED – to find those patients with structural disease.)
A few more studies
Aldous S, Richards AM, Cullen L, Pickering JW, Than M. The incremental value of stress testing in patients with acute chest pain beyond serial cardiac troponin testing. Emergency medicine journal : EMJ. 2015. PMID: 26511125
- Prospective observation trial of 1483 patients with negative biomarkers. 749 underwent stress test (so there were somewhat selective – not everyone needs this test.
- Stress testing identified 32 “true positives” only 22 of which had a stenosis greater than 70%
- Very low yield (4.3%), but more importantly – the only benefit they claim is that these patients got revascularization. However, as you know from above, in these patients with negative biomarkers, there is no benefit to revascularization
Napoli AM. The association between pretest probability of coronary artery disease and stress test utilization and outcomes in a chest pain observation unit. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 21(4):401-7. 2014. PMID: 24730402 [free full text]
- Prospective observational trial of all chest pain patients at a single center
- Over 2 years, 3543 patients were admitted for observation for chest pain
- 1754 patients with negative biomarkers underwent stress test, with 20 true positives. And again, the only change in their management would be an unnecessary cath
Bottom line
It is worth knowing that others (just not the writers of guidelines) have noticed this literature. As a surrogate for my bottom line, I will quote from a review on the subject in Emergency Medicine Clinics of North America:
Kosowsky JM. Approach to the ED patient with “low-risk” chest pain. Emerg Med Clin North Am. 2011;29:(4)721-7, vi. PMID: 22040703
“Although American College of Cardiology/American Heart Association guidelines recommend that [low risk chest pain] patients “may be considered for an early stress test to provoke ischemia.[and] to assess for obstructive CAD,” there is no randomized-trial evidence to support this as universal practice.”
“For one thing, once a patient has “ruled out” for MI with serial biomarkers, the likelihood of an important ACS-related outcome (eg, STEMI, cardiac death) is exceedingly low, so that further risk stratification is inherently difficult.”
“Overall, the sensitivity (68%) and specificity (77%) of ETT for CAD is limited, with even lower performance in women.”
“Whether there is a role for further risk stratification with provocative testing and/or coronary imaging before discharge remains open to debate.”
Morgenstern, J. EBM Lecture Handout #4: Stress Testing (part 2), First10EM, June 16, 2015. Available at:
https://doi.org/10.51684/FIRS.519