There are a lot of recurrent themes in this month’s edition of the articles of the month (which has clearly shifted from being a monthly to a bimonthly publication). Podcast over on BroomeDocs.
Our lack of droperidol is going to make me puke
Braude D, Soliz T, Crandall C, Hendey G, Andrews J, Weichenthal L. Antiemetics in the ED: a randomized controlled trial comparing 3 common agents. The American journal of emergency medicine. 2006; 24(2):177-82. PMID: 16490647
There have been a few articles recently indicating that none of the anti-emetics we use in the emergency department seen to provide better outcomes than placebo. I include this article to remind us that we used to have an agent that worked: droperidol. This randomized, double-blind, placebo controlled trial compared 1.25 mg of droperidol, 10 mg of metoclopramide, 10 mg of prochlorperazine, and placebo (all intravenously) in 181 adult patients with moderate to severe nausea. The primary outcome was nausea at 30 minutes. Metoclopramide and prochlorperazine fared no better than placebo (with reduction of 41mm, 40mm, and 39mm respectively on a 100mm VAS). Droperidol was the lone agent better than placebo (55mm reduction (p=0.04). Droperidol did result in more restlessness. Almost all patients were satisfied with the medication they received. The study isn’t perfect, being small in size and only looking at 30 minute outcomes, but droperidol is the winner if you want to decrease nausea.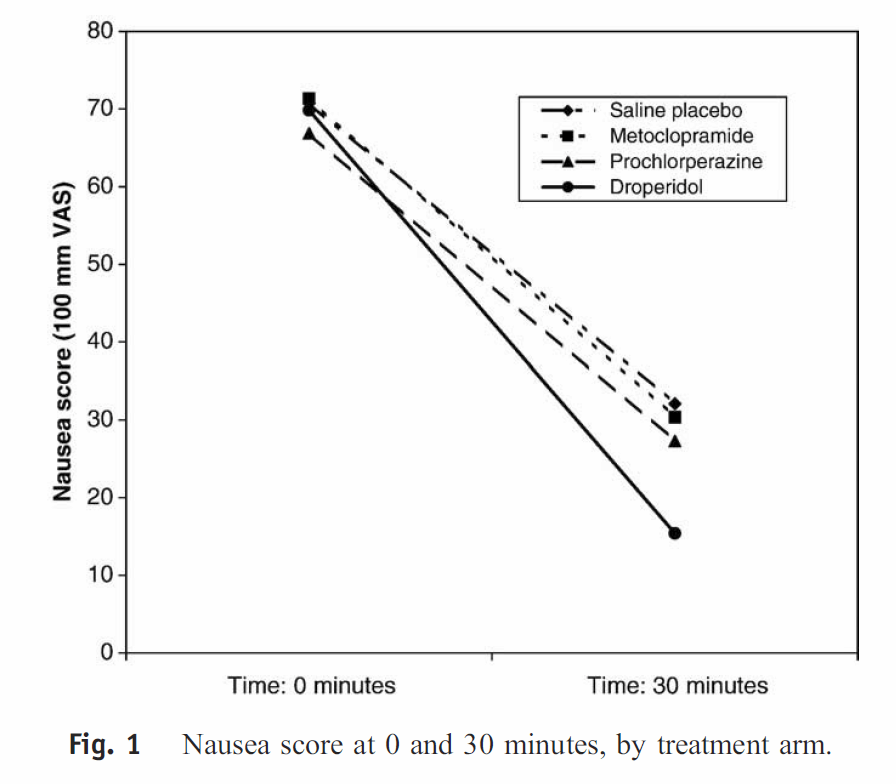
Bottom line: We really need to get our acts together and get droperidol back in our emergency departments.
A droperidol alternative?
Roldan CJ, Chambers KA, Paniagua L, Patel S, Cardenas-Turanzas M, Chathampally Y. Randomized Controlled Double-blind Trial Comparing Haloperidol Combined With Conventional Therapy to Conventional Therapy Alone in Patients With Symptomatic Gastroparesis. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2017. PMID: 28646590 [full text]
If you don’t have droperidol, you need an alternative for patients with vomiting. I covered haloperidol as an option last month, but this RCT strengthens that retrospective data. This is a double-blind, RCT that included 33 patients with previously diagnoses gastroparesis who presented to the emergency department with vomiting. They compared haloperidol (5mg IV) to placebo. Patients would receive whatever other conventional therapies their treating physician thought was appropriate. Abdominal pain decreased from 8.5 to 3.1 (p<0.001) with haloperidol as compared to 8.3 to 7.2 (p=0.11) with placebo. Nausea decreased from 4.5 to 1.8 with haloperidol (p<0.001) compared to 4.1 to 3.4 with placebo (p=0.05). Fewer patients were admitted to hospital in the haloperidol group (27% vs 72%, p=0.009). Median length of stay was statistically unchanged, but the point estimate was shorter in the haloperidol group (5 vs 9 hours, p=0.77). There were no adverse events. Obviously, this study is limited due to its very small size. They measured pain and nausea at 1 hour, but we might care about longer term outcomes as well. I am not sure why they limited enrollment to patients with known gastroparesis, when we see so many patients with undifferentiated cyclic vomiting syndrome in the emergency department. They did ECGs on everyone to look for long QTs, but I am aware of no evidence that that is a helpful practice, but plenty of evidence that these medications are very safe in single dose settings.
Bottom line: Until someone brings droperidol back to Canada, haloperidol will remain a key component of my cyclic vomiting management strategy.
I hear Lance Armstrong has never had a sore throat
Sadeghirad B, Siemieniuk RAC, Brignardello-Petersen R. Corticosteroids for treatment of sore throat: systematic review and meta-analysis of randomised trials. BMJ (Clinical research ed.). 2017; 358:j3887. PMID: 28931508 [free full text]
I have been using steroids for patients with severe pharyngitis for years, but there has always been some debate about the practice. This is a systematic review and meta-analysis that includes 10 RCTs covering 1426 patients looking at steroids for sore throat. The most common treatment was a single dose of dexamethasone up to 10 mg orally. Patients given steroids were twice as likely to have pain relief at 24 hours (relative risk 2.2, 95% CI 1.2 to 4.3; ARR 12.4%). Complete resolution of symptoms at 48 hours was also higher with steroids (RR 1.48, 95%CI 1.26 – 1.75; ARR 20%). Other important outcomes were measured, such as time off work or school, antibiotics use, and recurrence, and although point estimates all favoured steroid use, the numbers are small enough that these comparisons were not statistically significant. There is no reported difference in adverse events, but these trials are too small and not designed to really give us a clear idea of harms. Steroids are not without harm, but major and minor, but there is a clear benefit here with a number needed to treat between 5 and 8. I don’t use steroids for everyone, but when patients are truly miserable this is clearly worth a shared decision conversation.

Bottom line: Steroids will decrease pain from pharyngitis, although the exact balance of harms and benefits is unclear.
On the other hand, Lance has had some other problems
Waljee AK, Rogers MA, Lin P. Short term use of oral corticosteroids and related harms among adults in the United States: population based cohort study. BMJ (Clinical research ed.). 2017; 357:j1415. PMID: 28404617 [free full text]
Let’s tackle the other side of steroids: harm. This paper has received a fair amount of press, although I am not sure it warrants the attention. This is a retrospective look at a massive insurance database in the United States. Patients over 65 were excluded because they have Medicare, and so wouldn’t be captured. You also had to have coverage continuously for the 3 year study period. (In other words, this is a select population that might not include patients at the highest risk for adverse events). They were looking at patients who used a short course of oral corticosteroids (less than 30 days over the 3 years), and tried to get at first time users by excluding patients who filled a prescription for steroids in the year prior to the study period. They focused specifically on 3 harms (although they weren’t too clear about the rationale for focusing on just these 3): sepsis, venous thromboembolism, and fractures. There were 1,548,945 adult patients in the database, of which 327,452 (21%) received at least one outpatient prescription for oral steroid over the 3 year period. (That is an insanely high number, in my opinion.) There was an association between oral steroid use and all of sepsis, VTE, and fractures. However, it is really hard to know what that information means. This is a retrospective association. The group that was given steroids was, not surprisingly, older and had more comorbidities – exactly the kinds of patients you would expect to get sepsis, VTE, and fractures. They do say that even in the same patient, risk is higher in the period immediately after the steroid prescription, but I think that is also pretty meaningless information. Steroids were prescribed because the patient was sick, so to point out that they had complications while they were sick borders on meaningless. Furthermore, if you look at the absolute number they are talking about (2 in 1,000 risk of sepsis over a year, 5/1,000 VTE, and 21/1,000 fracture) it isn’t clear any of this has much clinical significance. So overall this is a tenuous association with tiny numbers. It shouldn’t worry us and this study really didn’t warrant the kind of press it got. However, this study was not looking at all harms. For some reason they ignored the more common GI and psychiatric side effects. We know steroids have side effects. We should never use any medication that isn’t going to help. However, when compared to the relatively large symptomatic benefits we see from using steroids for conditions like severe pharyngitis, the benefits will almost certainly outweigh the harms for most patients.
Bottom line: We know there are adverse events from steroid prescriptions, but this study really doesn’t give us much information.
Red hot guideline on gout
Qaseem A, Harris RP, Forciea MA. Management of Acute and Recurrent Gout: A Clinical Practice Guideline From the American College of Physicians. Annals of internal medicine. 2017; 166(1):58-68. PMID: 27802508
This is a well done clinical practice guideline (meaning transparently based in evidence) with a few decent take homes about gout for emergency practitioners:
-
- NSAIDs, corticosteroids, and colchicine are all reasonable options in acute gout. (Colchicine is generic, but still more expensive than the other 2 options).
-
- All NSAIDs are probably equally effective. (16 moderate quality RCTs)
-
- When comparing steroids and NSAIDs, there is no difference in time to resolution of symptoms, but NSAIDs have higher rates of GI side effects and serious adverse events. (6 RCTs)
-
- If colchicine is chosen, use a low dose regimen (1.2 mg PO once, followed by a single 0.6mg dose 1 hour later).
-
- They recommend against starting long-term urate lowering therapy after a first gout attack or in patients with infrequent attacks.
- In terms of diet recommendations, giving general advice on weight loss and reducing alcohol intake seems to be as effective as specific diet advice (such as reducing intake of red meat, shellfish, and yeast-rich foods and increasing intake of low-fat dairy products, vegetables, and cherries). (Based only on 1 RCT).
Rant of the month: Stop blaming patients
Callaham ML. The Prudent Layperson’s Complicated and Uncertain Road to Urgent Care. Annals of emergency medicine. 2017. PMID: 28935282
In emergency medicine, there is a constant debate about patients who are “inappropriately” using the emergency department. There was some heated Twitter debate last month when I tweeted: “Every single person who comes in to the emergency department thinks they are having an emergency. They are scared. You can always help.” This article was brought up by Seth Trueger in the context of that debate. They run through a number of evidence based reasons that we should not be blaming patients for choosing the emergency department. First, many of these patients were specifically told to come the the emergency department. They were referred in, or they called their physician’s office, and the secretary told them to go to the ED. Second, it is unreasonable to us to expect patients to be able to accurately assess the severity of their condition. The most common “non-urgent” chief complaints, such as fever, are also the among the most common “urgent” chief complaints. Even when using validated algorithms or trained triage personnel, a significant percentage of patients categorized at low acuity end up getting urgent treatment, surgery, or being admitted. If we, as trained professionals, can’t accurately triage patients, how can we expect our patients to accurately triage themselves? Even if we could expect patients to accurately triage themselves, we have to recognize the paucity of evidence comparing quality of care in different settings, the lack of access to alternative care, and ability to pay (in some countries). I would add that although we like to blame low acuity patients for many of the problems facing emergency medicine, patients who require no testing or interventions require very little time to disposition and are unlikely to significantly influence a department’s efficiency. As for cost, ignoring the charges to patients in for profit health care, the emergency department needs to be staffed 24 hours a day, 365 days a year. If we have to pay for staffing anyway, seeing a few low acuity patients is probably an economic benefit. There are certainly patients who don’t need to be in the emergency department, such as the well child with 24 hours of fever. However, no one ever chooses to spend time in an emergency department for fun. They come to use because they are scared. Some patients are scared even though they don’t need to be, such as the parents of the child with 24 hours of fever. These patients need education, not user fees. Unfortunately, the current system relies on providing that education when it is already too late: when the patient is in the emergency department. This is an issue that requires a societal fix, with a greater emphasis on health education starting in our elementary school systems.
Bottom line: We need to stop blaming patients for using the emergency department. We have system issues and societal education issues that we need to address, but for now I am happy to look after any patient who is scared about their health.
An 11 blade and a side of Septra
Daum RS, Miller LG, Immergluck L. A Placebo-Controlled Trial of Antibiotics for Smaller Skin Abscesses. The New England journal of medicine. 2017; 376(26):2545-2555. PMID: 28657870
This is the second paper in the last year demonstrating some benefit from routine antibiotics for abscesses. (The previous one was covered here.) These results are pretty similar. This is a multicenter, double-blind, placebo controlled, RCT that included 786 patients (pediatrics included) with a small abscess (less than 5 cm). Patients were randomized to TMP-SMX (160mg/800mg BID), clindamycin (300mg TID), or placebo. Important exclusions were fever, SIRS criteria, and immunosuppression. Almost all abscesses were cultured, and the results confirm what we already know: abscesses are almost all caused by staph. Both antibiotic groups outperformed placebo, but performed similarly to each other (83% cure with clindamycin, 82% cure with TMP-SMX, and 70% cure with placebo). My big problem with both these studies is the 70% cure rate without antibiotics. That is really low as compared to what I am seeing. Part of that might be because of the higher rate of concomitant cellulitis (a mean of 27 cm2 in this study) which I don’t usually consider as a simple abscess. However, the definition of cure is also funny. There really wasn’t a difference in the cure of the of original abscess. The difference was basically all in new lesions at other sites, so we really might be talking about a decontamination therapy. Most importantly, these studies are using a sort of straw man comparison. No emergency physician I know never uses antibiotics for abscesses. We use clinical judgement, and prescribe antibiotics occasionally. Comparing antibiotics to usual care rather than placebo would be a much more convincing study. These studies clearly indicate that the old adage that all abscesses need is cold hard steel is wrong – some will benefit from antibiotics. However, I don’t think this means we should be using antibiotics for all patients. The benefit here is relatively small (more about inconvenient second lesions than life threatening infections) and we know antibiotics also cause many inconvenient side effects. My practice hasn’t really changed: I prescribe antibiotics for patients with abscesses, but only for high risk patients, recurrent abscesses, or if there is significant surrounding cellulitis.
Bottom line: Some patients will benefit from antibiotics after I+D of their abscess.
Quick update on the easy IJ
Gottlieb M, Russell FM. How Safe Is the Ultrasonographically-Guided Peripheral Internal Jugular Line? Annals of emergency medicine. 2017. PMID: 28969927
This is yet another topic I have covered before in these pages. This is a quick review that aimed to provide a summary of the current evidence about the efficacy and safety of placing ultrasonographically-guided peripheral internal jugular venous lines. They identified 5 studies, but those studies only include a total of 154 patients. There are no reported complications of this procedure in the literature, but because of the small size of the studies, this doesn’t translate into evidence for safety. I think here are patients that this will be a good, temporary rapid access line, but it will not be my routine first choice in patients with difficult access at this time.
Bottom line: The ability to rapidly (and safely) place a peripheral IV into the internal jugular could be lifesaving in the correct patient, but shouldn’t be used routinely.

Machine learning: friend or foe?
Cabitza F, Rasoini R, Gensini GF. Unintended Consequences of Machine Learning in Medicine. JAMA. 2017; 318(6):517-518. PMID: 28727867
This is an interesting commentary that discusses the tension between the inevitable introduction of machine learning into medicine with the incomplete, biased, and uncertain data on which we make our decisions. Diagnostic algorithms are going to come, but we have to be really careful about what they look like, the data they are based on, and how they are used.
Obermeyer Z, Lee TH. Lost in Thought – The Limits of the Human Mind and the Future of Medicine. The New England journal of medicine. 2017; 377(13):1209-1211. PMID: 28953443 [free full text]
Almost a rebuttal to the above paper, but just happened to come out at the same time in a different journal. Argues that modern medicine is becoming too complex and data dense for the human mind to be able to handle. We might be able to accurately read a single ECG, but we can’t possibly interpret every QRS complex from a 48 hours Holter monitor, or the endless tsunami of data coming from personal health devices. Machine learning is going to be necessary to handle all this data, and these authors present a more optimistic viewpoint of that future.
Cheesy Joke of the Month
Apparently all diarrhea is hereditary: it runs in your jeans.
Morgenstern, J. Article of the month (November 2017), First10EM, November 20, 2017. Available at:
https://doi.org/10.51684/FIRS.5179





2 thoughts on “Article of the month (November 2017)”